Using engineered immune cells to treat DIPG, a devastating brain tumor in kids
Diffuse intrinsic pontine glioma (DIPG), also known as diffuse midline glioma, is a devastating type of pediatric brain cancer. The tumor is very aggressive and located deep within the brain, making it difficult to treat. The majority of DIPG tumors are caused by a mutation called H3K27M. The 5-year survival rate for kids with DIPG has been 0% since the 1950s, so new treatments are desperately needed. Donor support is enabling researchers to search for those new treatments.
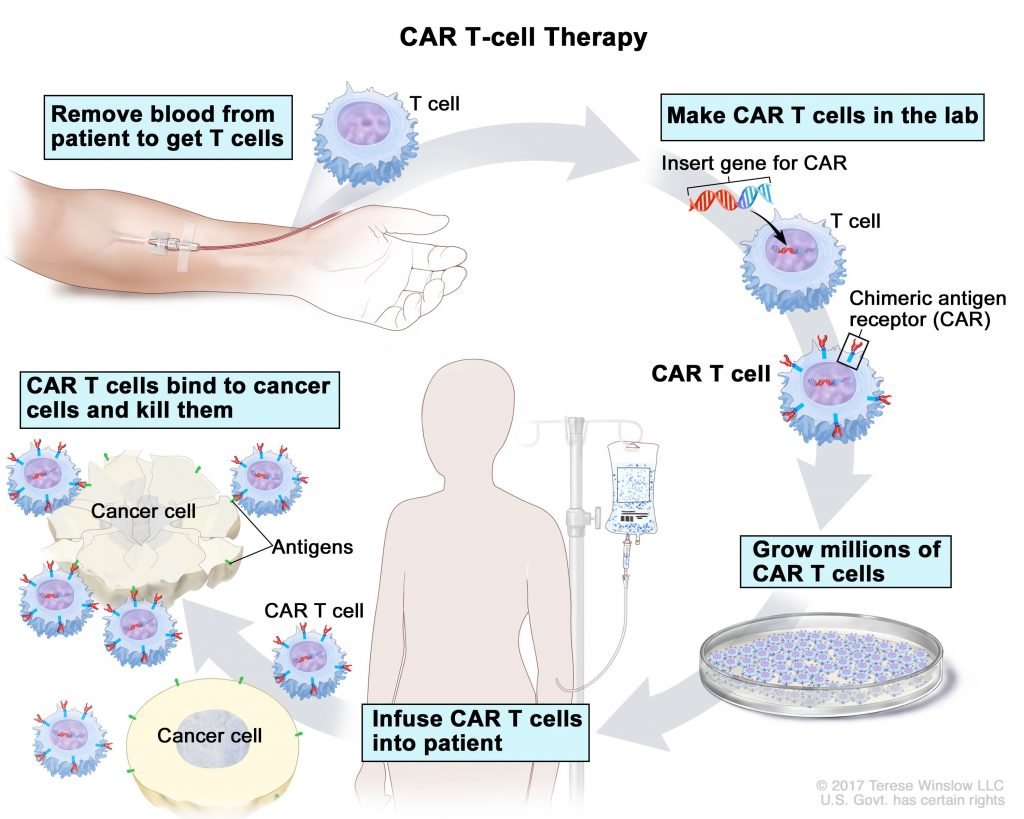
Immunotherapy is a type of biological therapy that utilizes the patient’s immune system to fight cancer. Over the last decade, immunotherapy has been proven as an effective treatment for a range of cancers. One form of immunotherapy, called CAR T cell therapy, has shown a high level of success for leukemia and lymphoma patients, so the researchers you support are expanding into other forms of pediatric cancer, including DIPG and other types of brain cancer.
CAR T cell therapy reprograms a patient’s T cells (the immune cells that protect the body) so that they will attack cancer cells. A CAR T cell is created by adding a new receptor to the surface of the patient’s T cells. That receptor is called a chimeric antigen receptor, or CAR. Combining the CAR with the patient’s T cells results in a CAR T cell. Once created, the patient’s new CAR T cells are returned to their body through an infusion where they will target and attack the cancer cells. The CAR T cells do this by latching onto the antigens on the surface of the tumor cells and killing them.
The first step in creating an immunotherapy treatment is identifying the critical antigen(s) that are present on the surface of the cancer cells. Dr. Sujatha Venkataraman and other researchers in Dr. Rajeev Vibhakar’s lab have identified two such antigens that are present on the surface of H3K27M DIPG tumor cells.

In collaboration with Dr. Mark Kohler, Dr. Venkataraman has developed novel CAR T cells targeting each of the antigens. These CAR T cells have completely killed DIPG cells in lab cultures and in vivo models. While this is very encouraging, additional steps need to be taken because the two antigens present on DIPG cells can also be found on normal human cells. That means the novel CAR T cells the researchers created would potentially also target and kill the patient’s normal cells.
Avoiding this potential problem required a highly innovative idea from the research team. They have engineered an even more advanced CAR T cell that follows a logic function so that it will only attack and kill cells that possess both antigens. DIPG tumor cells have both of the two identified antigens on their surface, but normal cells only have one antigen or the other. That means the logic-gated CAR T cells should ignore the normal cells and only latch onto the cancer cells.
The researchers tested the logic-gated CAR T cells and confirmed that they work as expected and kill only the tumor cells and not normal cells. This is an innovative and encouraging success in CAR T cell engineering. Several CAR T cell therapies developed in other labs have ended in failure because the CAR T cells attacked the normal cells as well as the cancer cells.
Now that the logic-gated CAR T cells are ready to go and their efficacy has been confirmed in the lab, the researchers are expanding their in vivo testing in DIPG tumors. The team expects that the novel logic-gated CAR T cells will show rapid tumor regression while protecting the normal cells. This testing is the next step in the process to prove that this approach is viable for treating kids with DIPG.
This work is ground-breaking research in DIPG utilizing immunotherapy, a relatively new approach that has been called the “fifth pillar” of cancer treatment. Currently, the standard treatment for DIPG is radiation, but it is not curative and merely extends the child’s life.
Being able to treat kids with this uniformly fatal brain tumor using immunotherapy would be a monumental improvement. Your generous support will help researchers take this novel CAR T cell therapy from bench to bedside to treat kids with DIPG. Donate now!
Families of children diagnosed with DIPG have been without hope for decades; this project is an important step toward improving the outcomes of kids with DIPG.