Neurofibromatosis Type 1 (NF1) is an inherited genetic disorder that leads to the formation of tumors on the peripheral nervous system, called plexiform neurofibromas. Plexiform neurofibromas are often benign, but they can transform into fatal malignant peripheral nerve sheath tumors (MPNST).
Plexiform neurofibromas typically develop during childhood and early adulthood. They occur in various parts of the body and are often very painful and disfiguring. NF1 affects 1 in 3,000 people at birth, making it one of the most common inherited genetic mutations.
Ten percent of patients with plexiform neurofibromas go on to develop malignant peripheral nerve sheath tumors. MPNST is an aggressive cancer with a very low survival rate. It is the leading cause of death for people with NF1.
Little is known about the underlying tumor biology of plexiform neurofibromas and MPNSTs, so treatment options are limited.
Surgical resection is the standard of care, but due to the tumors’ highly infiltrative nature, they are often inoperable. When surgery is possible, recovery is extremely painful, and residual areas of tumor can be left behind. Chemotherapy and radiation treatment have not shown benefits for patients.
Dr. Nick Foreman is the director of the Neurofibromatosis Therapeutic Program at Children’s Hospital Colorado.
In 2020, researchers in Dr. Foreman’s lab began studying the two types of tumors found in NF1 patients. The goal of the work was to gain an understanding of how plexiform neurofibromas tumors transform into more aggressive and lethal malignant peripheral nerve sheath tumors.
It was the first time cutting-edge single nuclei RNA sequencing had ever been completed on NF1-associated tumors.
This first-of-its-kind work to identify and describe subpopulations of cells in plexiform neurofibroma and MPNST yielded important new knowledge. Both tumor types have a complex variety of tumor cells with some clear differences.
Malignant peripheral nerve sheath tumors have unique subpopulations of cells compared to plexiform neurofibromas. This is important because even though MPNSTs arise from plexiform neurofibroma tumors, the process of transformation is extremely complex and not very well understood.
Because of MAF donor support, Dr. Foreman’s team continued the work in 2021 and 2022.
The use of a state-of-the-art technology called Visium allows the newly identified cell types within plexiform neurofibroma and MPNSTs to be mapped back to their relative positions within the body of the tumor.
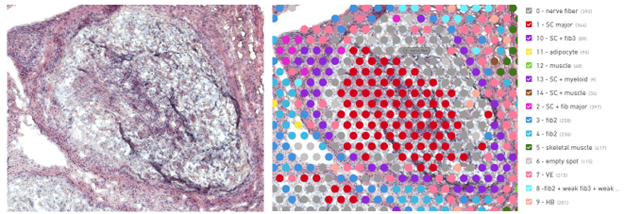
Visium data integrated with single-cell analysis provides a greater understanding of the cell-to-cell interactions that drive disease progression. Researchers have been able to follow the mechanisms of transformation from plexiform neurofibroma to MPNST and identify critical signaling pathways that may be targetable with new treatments.
The research team now has viable MPNST cell lines to test treatment options in the laboratory. This is a critical step toward getting a new treatment into a clinical trial.
Doctors have a good idea which NF1 patients are going to get MPNST, and these tumors can cause death within a matter of weeks. According to Dr. Foreman, stopping the transformation of plexiform neurofibromas into MPNSTs at this stage is the ultimate goal of his laboratory studies.
The Foreman Lab