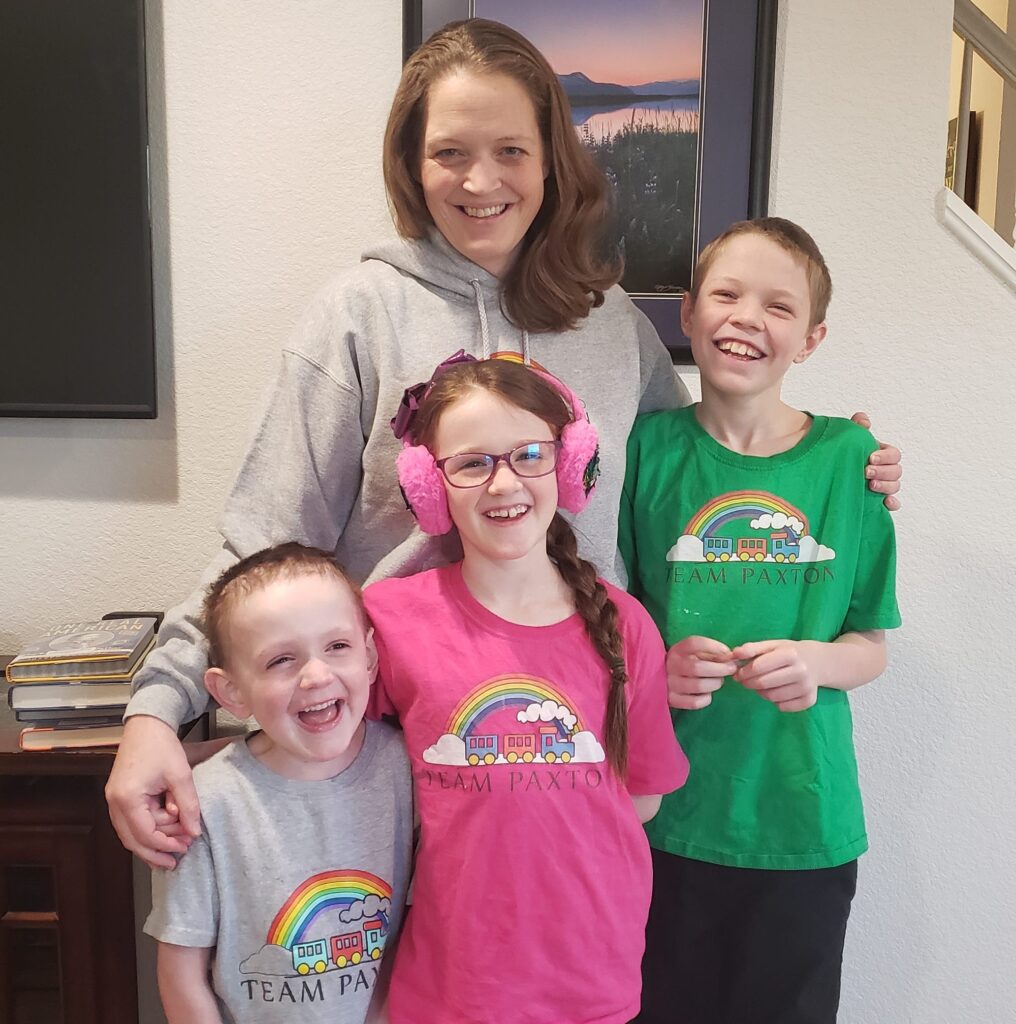
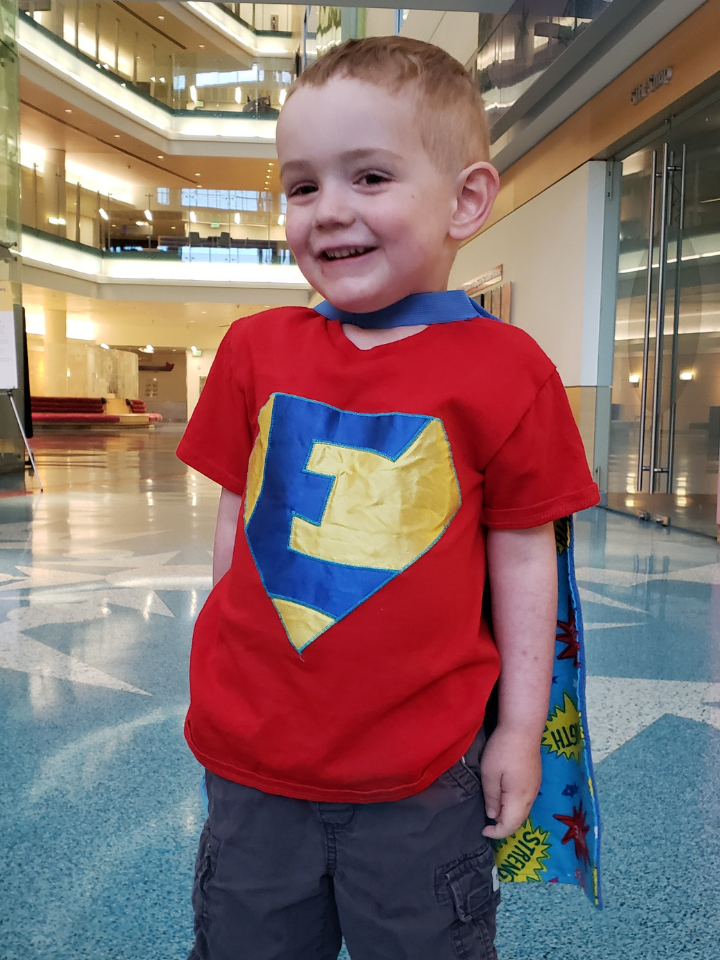
Eli M.
Below is Eli’s medical story of his battle with brain cancer. Although Eli battled cancer for most of his life; he never let cancer define his life. Eli wanted people to know three things about cancer: it takes a lot of time, it is hard to treat, and it sucks. Eli was one of the toughest kids we have ever met. He died from cancer on October 14, 2022, and was living his best life up until that day.
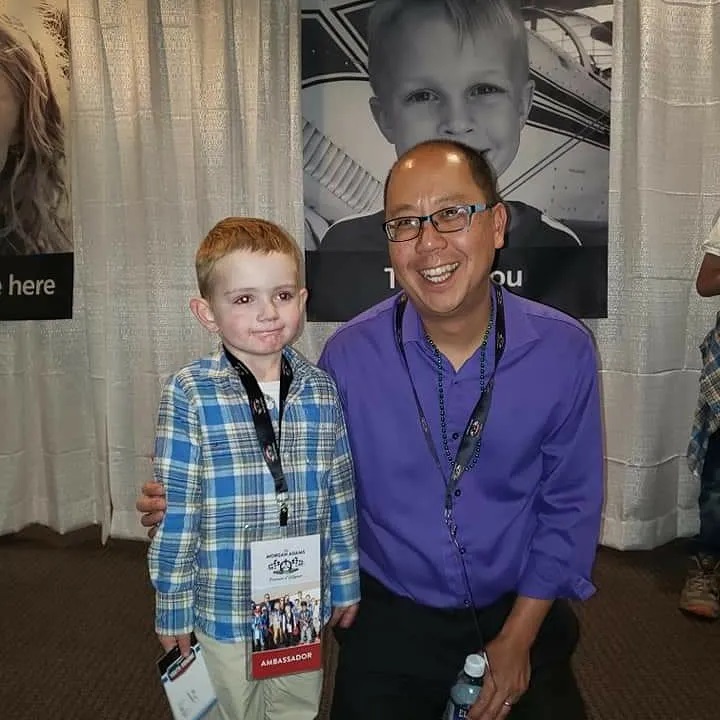
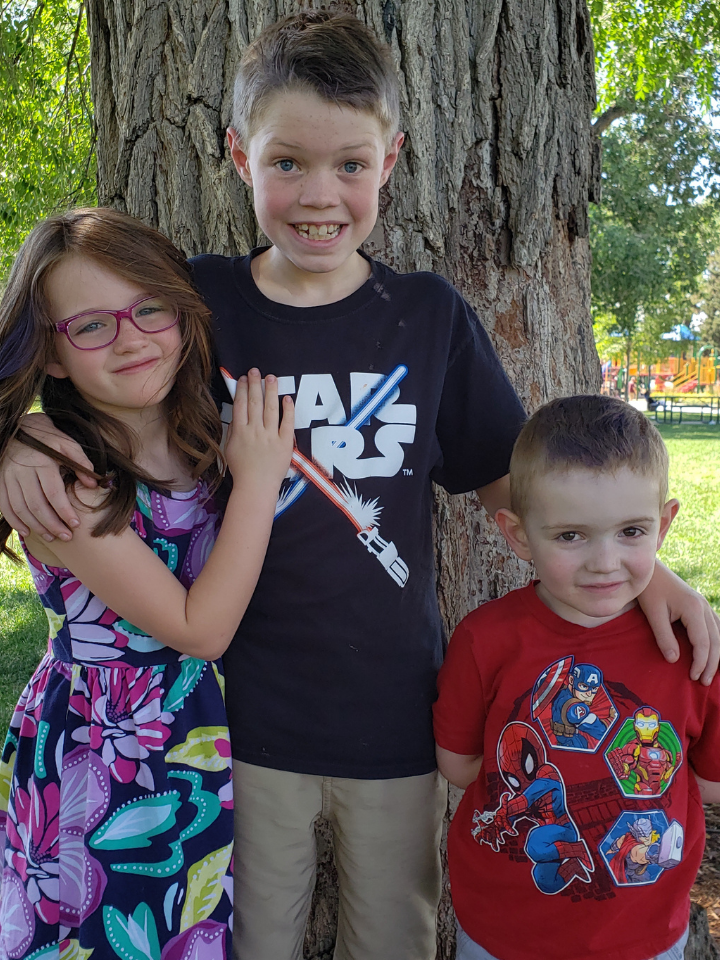
In his short time on earth, he lived a very full life with his determination, joy, courage, and desire to enjoy everyday memories. Even with all the challenges Eli faced, he learned to downhill ski. He prided himself in being able to ski black diamonds and speed down mountains. He played soccer and learned how to ride a bike. Eli loved the outdoor; camped and hiked up mountains. He traveled to 32 different states in the US and Canada. He enjoyed hiking in the Grand Canyon, explored different sea life animals in Alaska, swam in the ocean and watched an epic sunset in Hawaii, and enjoyed a sunrise on Cadillac mountain in Maine. Eli loved to run and achieved his goal of making it onto the mile run wall of fame for his school, having one of the fastest times among 1st graders for the fall of 2022. He loved school, learning, and reading. Eli was able to live this amazing life thanks to the efforts of The Morgan Adams Foundation to fund research and create possible treatment options when there wasn’t one.
In late March 2017, Eli was a lively, active almost 2-year-old when we noticed Eli was having problems moving his left arm. He was always playing and trying to keep up with his siblings, so we assumed he must have sustained a minor injury from everyday play. We followed up with a routine doctor’s visit for good measure. Eli’s doctor thought the same thing. However, a couple of weeks later when Eli was having trouble turning his neck, we took him to Children’s Hospital Colorado where an MRI revealed a mass that spanned from Eli’s brainstem down into his spine.
Eli underwent an extremely complex 11-hour surgery where doctors removed all they could of the tumor. Following surgery, Eli couldn’t lift his head or move the left side of his body. It was almost a week before he was able to walk again. Pathology reports shortly after indicated the tumor was a juvenile pilocytic astrocytoma (JPA). We were relieved to hear from doctors that Eli’s outlook was positive: he had a “good” type of brain cancer and there was a 90% chance the tumor would not come back.
In June of 2017, our relief turned to heartbreak when a follow-up MRI showed Eli’s tumor had grown by more than 50 percent. Doctors told us that the tumor was acting more like a high-grade glioma. They explained that our situation was grave and that there was no known treatment plan. Eli began radiation enduring 28 treatments over six weeks that required sedation each time. The radiation treatment led to hydrocephalus (the buildup of excess cerebrospinal fluid in the brain), which meant Eli went in for another surgery to relieve the pressure in his brain.
Eli’s neuro-oncologist, Dr. Nick Foreman, wasn’t satisfied with radiation as the only option, so during that six weeks of treatment, he and researchers in his lab analyzed Eli’s tumor and found that it harbored a rare genetic fusion called FGFR1-TACC1. From there, they screened Eli’s cells against more than 140 different FDA-approved drugs to determine which was most effective in killing the cancer cells. Trametinib, a MEK-inhibitor typically used for metastatic melanoma in adults, showed the best potential and was selected for Eli’s treatment. Eli took trametinib daily from October 2017 through September 2019. And then paused to give his body a break from treatment and see what might happen. He had almost 12 months of stable scans, but his cancer was sneaky and relentless. The tumor started growing again in August 2020 and started to spread.
We were again faced with the fact there was no known treatment protocol for Eli’s type of cancer. Eli was blazing a trail for himself and other kids with rare genetic mutations that make their types of cancer difficult to treat. In the fall of 2020, Eli was one of the first kids to try a combination of two inhibitor chemotherapy drugs that were created for adult cancers. Unfortunately, by Christmas of 2020, this option caused Eli to get really sick and he lost the ability to walk. We had to take a break from treatment to let his body heal. Amazingly enough, Eli had 8 months of tumor stability on his quarterly MRI scans while not needing any treatment. Unfortunately, our luck ran out in August 2021 when we learned that his cancer had spread to many locations in his brain. Eli started another chemotherapy cocktail which did slow the growth of the tumor. Sadly, there were no other options for Eli.
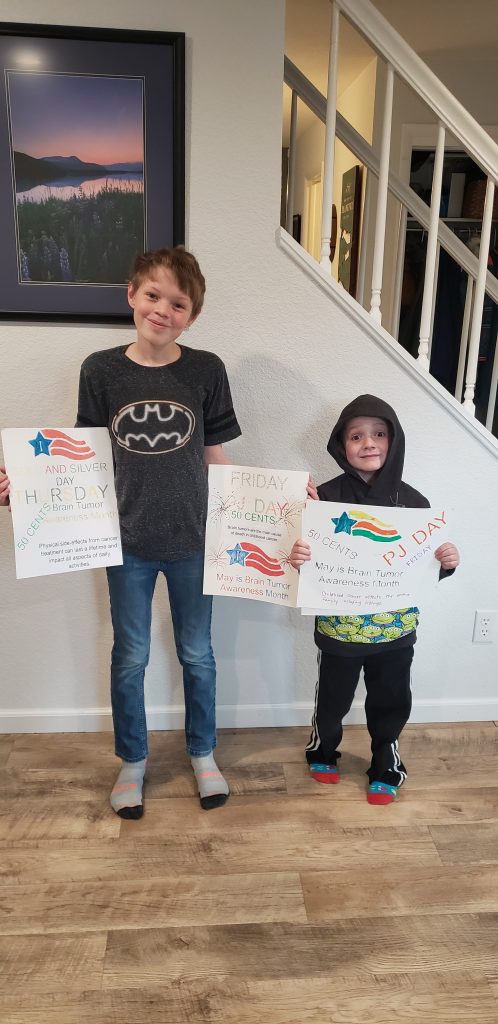
Eli was a fighter. To fight his cancer, he took almost 2,000 doses of oral chemotherapy, had 34 radiation treatments, 54 MRI scans, 218 therapy appointments (PT/OT), and 130 oncology appointments. We can change the narrative for childhood cancer and it starts with understanding the challenges and funding research.
Click here to make a gift to help kids with cancer in honor of Eli.